Redazione
|
19/12/2023 - Last update 19/12/2023
Valérie Attali, Olivier Jacq, Karine Martin, Isabelle Arnulf, Thomas Similowski | Year 2021
Osteopathic Manipulation of the Sphenopalatine Ganglia Versus Sham Manipulation, in Obstructive Sleep Apnoea Syndrom: A Randomised Controlled Trial
Pathology:
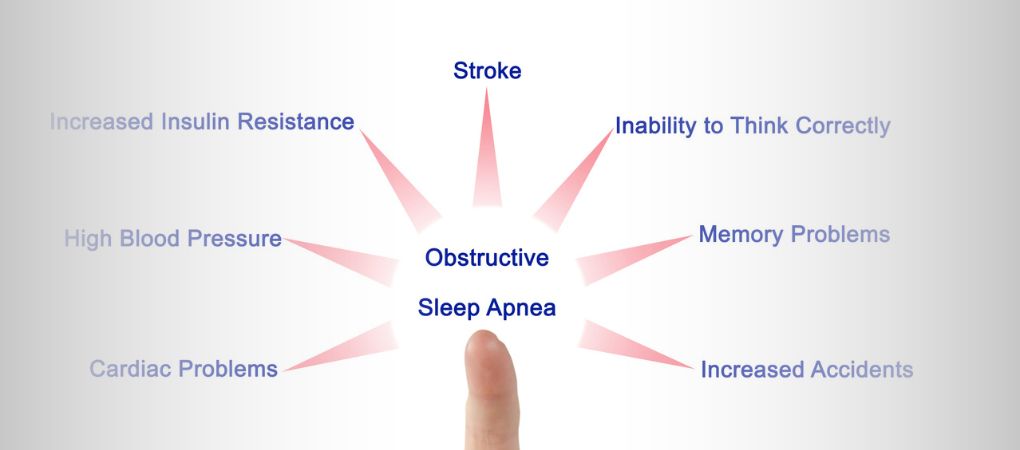
Obstructive sleep apnoea syndrome (OSAS)
Type of study:
Crossover Randomized Controlled Trial
Date of publication of the study’:
2021/Dec/24
Purpose of the study
- Objectives: to evaluate the effects of OMT on indices of respiratory efficiency and stability in people with moderate to severe obstructive sleep apnea syndrome (OSAS).
- Measured outcomes:
- Primary outcomes: Assessment of the apnea-hypopnea index (AHI).
- Secondary outcomes: Evaluation of peak nasal inspiratory flow (PNIF) and upper airway stability by measurement of critical closing pressure, while awake (Pcrit); sensations felt after treatment; adverse effects.
Participants
- Number: 30 people (6 female and 24 male, mean age 57 years).
- Criteria of inclusion: adults (age ≥18 years), with OSAS, AHI between 15/h and 45/h, body mass index ≤40kg/m2.
- Criteria of exclusion: pregnant women, nursing mothers, people with complete nasal obstruction, with a history of pharyngeal surgery and/or ongoing treatment with serotonin reuptake inhibitors.
- Groups of study: 2 groups obtained by randomization
- Group 1: OMT and then sham treatment, 14 people.
- Gruppo 2: sham treatment and then OMT, 16 people.
- Before the actual study, 20 healthy people (age between 18 and 40 years, low probability of OSAS according to Berlin score, body mass index < 30 kg/m2) had been analyzed according to the same randomized crossover design.
Interventions and evaluations
- Assessment of AHI by polysomnography at the beginning of the study, in the evening after the first treatment, 21 days after the first treatment, and in the evening after the second treatment.
- The following were also assessed: total sleep time; percentage staying in stages N1, N2, N3, REM of sleep; desaturation index; time spent with partial oxygen saturation (SpO2) <90%.
- Evaluation of nasal obstruction by measuring PNIF and Pcrit (defined as critical closing pressure) before, 30 minutes after, and 24 hours after each treatment.
- Evaluation at each intervention of induced pain by Visual Analog Scale (VAS), induced tearing in both eyes by Schirmer test – useful in assessing proper application of treatment – and sensations experienced by a brief interview (simple “Yes/No” questions).
- 1 OMT session and 1 sham treatment session 28 days apart, directed at the sphenopalatine ganglion.
- The treated person had to open their mouth and turn their head to the opposite side from the treated ganglion.
- OMT: pressure applied with the little finger of the hand in the pterygopalatine fossa toward the sphenopalatine ganglion, first to the right and then to the left.
- Sham treatment: insertion of the finger in the mouth as during OMT, but without touching the pterygoid process and applying pressure to the jaw.
- Patients treated with CPAP or mandibular advancement devices were asked to discontinue treatment in the 7 days prior to polysomnography.
- 6 failed to discontinue their treatment but were still analyzed in the study.
- Treatment applied by an osteopath who did not carry out any of the evaluations; evaluations performed by a physician blind to the treatment the patients would receive.
Results
- Primary outcomes: OMT did not appear to induce a greater decrease in AHI in comparison with sham treatment.
- Secondary outcomes: both 30 minutes later and 24 hours after treatment, OMT induced a statistically significant increase in PNIF compared to sham treatment. The latter, in fact, only induced a slight decrease or no effect at all.
As for Pcrit, the analysis was carried out on only 21 patients because of noncompliance during measurement in 9 people. It showed a slight decrease with OMT compared to sham treatment – lower Pcrit implies greater airway stability – although statistical significance was not reached. - Further analyses: both pain and tearing were higher after OMT than after sham treatment, reaching statistical significance. Similarly, after OMT all patients felt at least one sensation (nociceptive, tactile, olfactory, gustatory, auditory, or visual), while few people experienced similar effects after sham treatment. 8 people felt a bloody sensation in the mouth despite the absence of wounds.
After OMT, several people reported breathing better through the nose, while one reported feeling nasal obstruction. Fifteen patients noted changes in perceived position of mandibular or temporomandibular joints.
There were no differences in the other measured parameters (total sleep time; percentage staying in the N1, N2, N3, REM stages of sleep; desaturation index; time spent with SpO2 <90%). - Adverse effects: no adverse effects were observed during the study. Four people reported mild mandibular pain or discomfort 24 h after OMT.
- Analysis on the sample of healthy people: no differences in PNIF and Pcrit were found between OMT and sham treatment. The reported sensations were very similar to the experimental group of people with OSAS.
Discussion
Despite an improvement in nasal and upper airway airflow – an improvement comparable to the one achievable pharmacologically in cases of rhinosinusitis or nasal polyp – OMT did not induce any change in AHI in people with moderate to severe OSAS.
However, this is a result in accord with the literature, which shows that although treating nasal obstruction is a central element in OSAS, this does not result in improved OSAS. However, it does result in improved quality of life, less snoring, less need for and greater tolerance of CPAP use.
Unfortunately, the impossibility to test 9 out of 30 people (practically, one-third of the sample) on Pcrit prevents any evaluation of this parameter, which is unfortunate considering the encouraging results obtained by OMT in previous studies.
Taking a cue from the literature on pharmacological or surgical neuromodulation of the sphenopalatine ganglion, and from emerging sensations following similar interventions, it is conceivable that OMT acts via a postganglionic parasympathetic blockade, although an objective measurement is needed to test this hypothesis.
More studies would be needed to measure the effect of more treatment sessions.
The review of Osteopedia
By Marco Chiera
Strengths: calculation of sample size by effect estimation; good description of the study procedures and outcomes; interesting comparison with a group of healthy people; study continuing a pilot study done earlier in order to improve knowledge on a specific topic; qualitative evaluation with reference to the intervention, useful to help practitioners know what patients might be feeling and help them make sense of these feelings.
Limits: low sample size, especially given the many outcomes measured (although these were secondary and exploratory outcomes); in addition to focusing on a specific maneuver, the authors could have evaluated a broader treatment, since a cornerstone of OMT is individualizing treatments; it is not specified how adverse effects were analyzed.

Are you an osteopath?
Register and enjoy the membership benefits. Create your public profile and publish your studies. It's free!
Register now
School or training institution?
Register and enjoy the membership benefits. Create your public profile and publish your studies. It's free!
Register now
Do you want to become an osteopath? Are you a student?
Register and enjoy the membership benefits. Create your public profile and publish your studies. It's free!
Register now







