Francesca Galiano
|
29/08/2022 - Last update 29/12/2022
Donald R Noll, Brian F Degenhardt, Thomas F Morley, Francis X Blais, Kari A Hortos, Kendi Hensel, Jane C Johnson, David J Pasta, Scott T Stoll | Year 2010
Efficacy of osteopathic manipulation as an adjunctive treatment for hospitalized patients with pneumonia
Pathology:
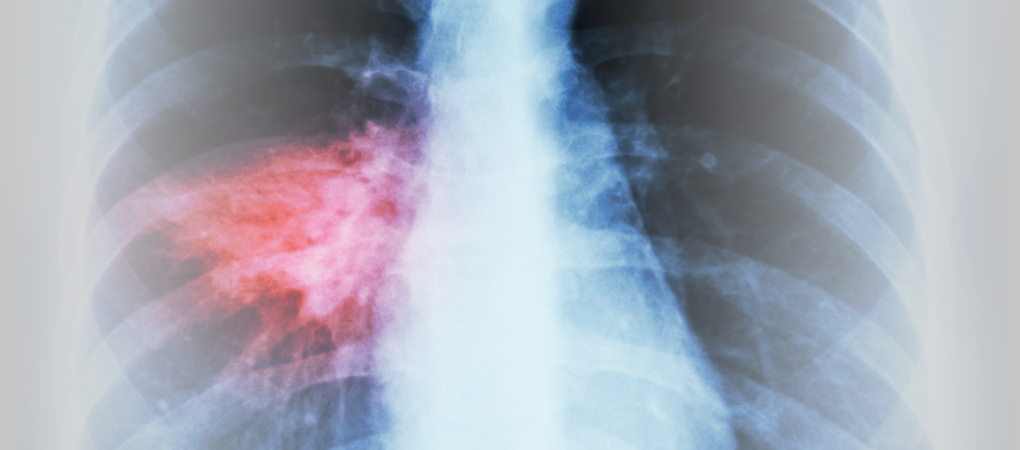
Pneumonia
Type of study:
Randomized controlled trial
Date of publication of the study’:
2010/Mar/19
Purpose of the study
- Objective: to evaluate the effects of OMT on pneumonia as an adjunctive treatment
- Measured outcomes:
- Primary: duration of hospitalization in days, time to achieve clinical stability, state of functional and symptomatic recovery
- Secondary: duration of oral or intravenous antibiotics therapies, treatment results, rate of new hospitalizations at 60 days, maximum daily body temperature, maximum daily respiratory rate, leukocyte counts, adverse effects
Participants
- Numbers: 387 people (213 female and 174 male)
- Criteria of inclusion: Criteria of inclusion: age ≥ 60 years (lowered to ≥ 50 years after 10 months from the beginning of the study), hospitalized with pneumonia with the appearance of a new pulmonary infiltration on chest x-ray and two of the following criteria: new or increase of cough, fever above 38°C, pleuritic chest pain, new physical finding on chest examination, respiratory rate greater than 25 breaths per minute, deteriorating mental or functional status, leukocyte counts more than 12,000 cells per mm3
- Criteria of exclusion: nosocomial pneumonia, lung abscess, advanced pulmonary fibrosis, bronchiectasis, pulmonary tuberculosis, lung cancer, metastatic malignancy, uncontrolled metabolic bone diseases, current vertebral or rib fractures, past fractures due to pathological conditions, respiratory failure
- Groups of study: three groups obtained by randomization
- Group 1: standard care with the addition of OMT, 130 people (71 female and 59 male, mean age 73.8 years)
- Group 2: standard care with the addition of sham treatment, 124 people (69 female and 55 male, mean age 74.6 years)
- Group 3: standard care, 133 people (73 female and 60 male, mean age 72.8 year)
- with a couple of exceptions, the groups did not differ for demographic or clinical aspects (eg, comorbidity)
Interventions and evaluations
- Evaluation of the severity of pneumonia measured upon admission to the hospital using pneumonia severity index
- Valuation of the duration of hospitalization as the difference between the discharge and admission dates
- Assessment of the time to achieve clinical stability as the day on which the following seven criteria were met:
- lowest systolic blood pressure ≥ 90 mmHg
- highest heart rate ≤ 100 heartbeats per minute
- highest respiratory rate ≤ 24 breaths per minute
- maximum temperature ≤ 38°C
- lowest oxygen saturation ≥ 90%
- capacity to eat by mouth or with the support of a feeding tube
- pre-pneumonia mental state
- Evaluation of the state of symptomatic and functional recovery through a validated questionnaire in relation to five symptoms: cough, dyspnea, sputum production, pleuritic chest pain and fatigue
- evaluation at the time of admission and subsequently on post-admission days 14, 30 and 60 via telephone calls (follow-up)
- Assessment of adverse effects as reports of the severity and type of muscle soreness, worsening of breathing or other adverse effects
- All people received standard of care for pneumonia
- 2 sessions per day of OMT or sham treatment from 15 minutes (at least 6 hours apart) up to:
- discharge, cessation of antibiotic therapy, respiratory failure, death or withdrawal from the study
- OMT: in sequence, techniques on thoracolumbar soft tissues, rib raising, doming of the diaphragm myofascial release, techniques on cervical spine soft tissues, suboccipital decompression, thoracic inlet myofascial release, thoracic lymphatic pump and pedal pump lymphatic techniques
- for the untreated areas, other techniques other than thrusts for an overall duration of less than 5 minutes
- Sham treatment: light touch modeled on the OMT (same zones, same sequence, same duration) but without activating biomechanical, circulatory or lymphatic responses (moving hands every 5 seconds, using contact zones close to those of the OMT, applying the forces more towards the bed, avoiding focused pressure with the hands)
- Protocol administered by 24 neuromusculoskeletal specialist osteopaths and 64 resident physicians in osteopathy
- phase of pre-study training on a standardized patient
Results
- Primary outcomes: the overall analysis found no statistically significant differences between the different groups. Whereas, excluding those people who, over time, no longer met the criteria of inclusion/exclusion, the group with the addition of OMT showed a greater reduction in the duration of hospitalization compared to the group with standard care alone (as a median, 3.5 days vs 4.5 days), but not compared to the group that received sham treatment.
A sub-analysis carried out by age showed that a reduction in hospitalization time occurred: with OMT, both for participants over 50 years of age and for those over 60 years of age; with sham treatment, only for people over 60 years of age. - Secondary outcomes: the overall analysis found no statistically significant differences between the different groups. While excluding over time those people who no longer met the criteria of inclusion/exclusion, the group with the addition of OMT showed a greater reduction in the duration of intravenous antibiotics usage, fewer episodes of death (0% vs 10%) and respiratory failure (1% vs 7%) and a lower respiratory rate than the group with only standard care, but not compared to the group that received sham treatment.
With regard to adverse effects, muscle soreness and pain were especially detected, mainly in the group with OMT, but only one person withdrew from the study because of them.
In the group with OMT there were three serious adverse effects, but not related to OMT. - Further analysis: a good part of the participants was not sure of knowing to which group they belonged, although about half of them was able to guess it.
Discussion
Analyses show that following the OMT properly (for example, participating in all sessions) results in different types of benefits (duration of hospitalization, use of antibiotics and severe comorbidities) in case of pneumonia, most likely primarily due to treatment-induced mobilization (immobilization is an important risk factor for pneumonia mortality).
Given that the sham treatment group had intermediate results compared to the other groups, we could conclude that OMT owes its effectiveness both to general touch reasons and to reasons related to the specific techniques used. This is especially true for younger people.
Studies are needed to assess the effects of the OMT also after discharge, mainly because: antibiotics continue to be administered also after discharge; compared to the past, hospitalization for pneumonia has been drastically reduced (from 2 weeks on average in the 90s to 5 days in 2010); several people were lost after discharge (e.g. did not answer the phone) preventing from properly assessing the symptomatic and functional status recovery.
The review of Osteopedia
By Marco Chiera
Strengths: very detailed description of the interventions (OMT and sham treatment), which makes them repeatable; phase of pre-study training; detailed description of the measured outcomes; in-depth discussion of the results, strengths and limitations.
Calculation of the sample size (how many people to recruit) on the basis of previous studies; evaluation of the degree of blindness of the recruited people (that is, if they understood or not to which group they had been assigned).
Statistical analyses applied according to both intention-to-treat (all persons are included in the analysis) and per-protocol (people who no longer meet the inclusion/exclusion criteria are excluded).
Limits: the use of a standardized treatment deviates from the clinical practice of OMT as a personalized treatment; given the reduced duration of hospitalization in case of pneumonia, the time of the study may have been too short to assess actual differences between interventions; many of the OMT sessions were performed by osteopathy students.

Are you an osteopath?
Register and enjoy the membership benefits. Create your public profile and publish your studies. It's free!
Register now
School or training institution?
Register and enjoy the membership benefits. Create your public profile and publish your studies. It's free!
Register now
Do you want to become an osteopath? Are you a student?
Register and enjoy the membership benefits. Create your public profile and publish your studies. It's free!
Register now







