Francesca Galiano
|
08/08/2022 - Last update 30/12/2022
Samir Kashyap, James Brazdzionis, Paras Savla, James A Berry, Saman Farr, Tye Patchana, Gohar Majeed, Hammad Ghanchi, Ira Bowen, Margaret Rose Wacker, Dan E Miulli | Year 2021
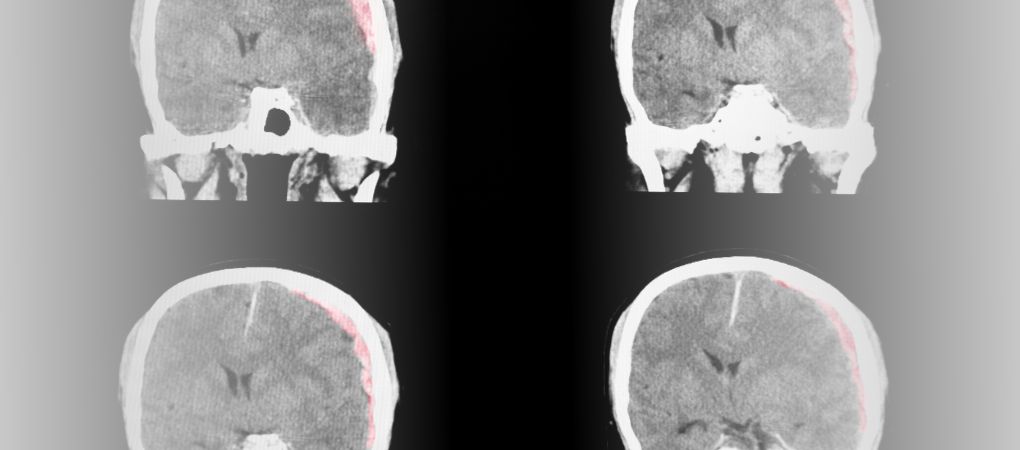
Osteopathic Manipulative Treatment to Optimize the Glymphatic Environment in Severe Traumatic Brain Injury
Pathology:
Severe traumatic brain injury
Type of study:
Retrospective study
Date of publication of the study’:
2021/Mar/11
Purpose of the study
- Objective: to assess the effect of OMT on glial lymphatic drainage in patients with severe traumatic brain injury, brain edema and elevated intracranial pressure
- Measured outcomes:
- Primary: intracranial pressure measured directly and with optic nerve sheath diameter and neurological pupillary index (NPi), parameters normally used in the management of the above mentioned pathologies
- Secondary: cerebrospinal fluid (CSF) drainage
Participants
- Number: 11 people
- Criteria of inclusion: adults (> 18 years); patients admitted to a Level II trauma center (severe emergencies) with severe traumatic brain injury (TBI), elevated intracranial pressure, cerebral edema or other situations requiring external ventricular drain.
- Criteria of exclusion: severe orbital-facial trauma, recent decompressive craniectomy, a history of ventriculoperitoneal shunt, any mass lesion requiring sanitary evacuation.
Interventions and evaluations
- All patients had an external ventricular drain placed to measure the flow of cerebrospinal fluid, and therefore the intracranial pressure, and to allow drainage
- Intracranial pressure, cerebrospinal fluid drainage and optic nerve sheath diameter were evaluated non-invasively with ultrasound, while the NPi was measured with pupillometry. All evaluations were carried out 1 hour before the OMT, at the beginning of treatment, 30 minutes after the start of treatment, 60 minutes after the start of treatment and for an hour once 30 minutes had passed since the end of the OMT
- Following the same timescales, the mean blood pressure, respiratory rate, systolic blood pressure and consciousness level on Glasgow Coma Scale were also measured (however, the results of these measurements were not reported)
- Standard of care including 1 session of OMT of 51 minutes structured as follow:
- 9 minutes of thoracic inlet opening
- 9 minutes of rib raising
- 9 minutes of diaphragmatic release
- 6 minutes of thoracic or pedal pump
- 9 minutes of compression of the fourth ventricle
- 9 minutes of facial effleurage facciale
- Each person was allowed to receive up to 3 treatments of OMT
Results
- Primary outcomes: the OMT favored a reduction in the optic nerve sheath diameter and an increase in NPi, both results indicate a decrease in intracranial pressure. All these effects have reached statistical significance.
- Secondary outcome: after the OMT, the drainage of the cerebrospinal fluid measured through external ventricular drain was lower than its pre-treatment levels. During OMT the drainage of cerebrospinal fluid increased slightly, but not in a statistically significant sense.
Discussion
A standardized OMT protocol has reported positive effects on lymphatic drainage in emergency conditions, namely TBI.
The intracranial pressure had a statistically significant decrease after the OMT compared to its level prior to the treatment, as both were measured according to the standard but invasive methodology of external ventricular drain – this tool is used to drain the cerebrospinal fluid accumulated inside the skull due to TBI – and non-invasive methodologies, such as, the assessment of the optic nerve sheath diameter and NPi – the optic nerve and the pupil are immediately affected by changes in intracranial pressure.
Of particular relevance was the decrease of the optic nerve sheath diameter as its average value went from abnormal (> 6mm) to normal (< 6mm) afollowing the OMT.
The post-OMT decrease in the cerebrospinal fluid drainage, in combination with a decrease in intracranial pressure, suggests the ability of the OMT to promote circulation and drainage of the liquor at the intracranial level.
Probably, the techniques used allowed the cerebral glymphatic system to drain the excessive liquor into the lymphatic circulation directed towards the thorax and, therefore, towards the rest of the body.
In this regard, the authors hope for future studies assessing the presence of specific biomarkers related to TBI, before and after OMT, so as to have more precise indications on the effects of osteopathy.
The review of Osteopedia
By Marco Chiera
Strengths: the use of non-invasive methodologies to assess the effect of OMT on intracranial pressure; the use of a standard OMT protocol, which allows easy replication for future studies; the study joins other previous studies in showing, at least in the acute care, the safety of the OMT in patients with concussion or TBI, even severe.
Limits: a small sample of people examined, all of them from the same trauma center; no measurements were carried out long-term, but only in the immediate period, which makes it impossible to determine whether the OMT had effects (or adverse effects) over time; the statistical analysis carried out was not described and, therefore, the results reported as significant, from a statistical point of view, may actually not be so.

Are you an osteopath?
Register and enjoy the membership benefits. Create your public profile and publish your studies. It's free!
Register now
School or training institution?
Register and enjoy the membership benefits. Create your public profile and publish your studies. It's free!
Register now
Do you want to become an osteopath? Are you a student?
Register and enjoy the membership benefits. Create your public profile and publish your studies. It's free!
Register now







